
We cannot achieve an end to AIDS by 2030 without addressing mental health challenges faced by young people living with HIV globally.
We have come a long way in the global response to HIV with world leaders working to end AIDS by 2030 under the Sustainable Development Goals. But we cannot do this without addressing the mental health challenges faced by people living with HIV.
Young people living with HIV often have worse treatment outcomes when compared to adults. Services are not youth friendly and the needs of young people, including their mental health needs, are often neglected. Consequently, over 30% of new HIV diagnoses occur among 15-25 year olds, and AIDS-related illnesses are the second leading cause of death for young people aged 10-24 globally.
Global survey on mental health among young people living with HIV.
Earlier this year Youth Stop AIDS and researchers at Newcastle University conducted research into mental health and young people living with HIV in partnership with Fundación Chile Positivo, Teenergizer, and Y+ Global. The research was funded by the Newcastle University Social Justice Fund. To read full report click HERE.
With research specifically on young people lacking, this survey was a crucial opportunity to hear the voices and experiences of young people living with HIV in order to understand how best we can address the mental health issues that they face.
Who took part in the survey?
We shared the survey with young people living with HIV and people who work directly with young people living with HIV including researchers, advocates, activists, NGO staff and health workers globally. 214 people responded spanning Africa, Latin America, Europe, Western-Pacific and South-East Asia*.
While the survey results were not representative of all young people living with HIV, and we had a lot more data from some regions than others, there were key similarities across countries and regions relating to the mental health challenges faced by young people living with HIV**.
What did young people living with HIV have to say?
![2[1]](https://youthstopaids.org/wp-content/uploads/2020/10/21-300x300.png)
![3[1]](https://youthstopaids.org/wp-content/uploads/2020/10/31-300x300.png)
![4[1]](https://youthstopaids.org/wp-content/uploads/2020/10/41-300x300.png)
For young people who did engage with mental health services, they played a vital role in facilitating access to mental health services of peers struggling to accept their diagnosis: “I was able to help a peer get linked to one of the support groups to help him to adapt to his status and include in our community.” (Young person living with HIV, Africa)
Young people also played a major role in delivering mental health services. Engaging in youth-led group or peer support, mentoring, or counselling was reported by 40% of young people living with HIV and by 60% of the people who work with them.
Alongside only 15% of young people feeling confident about disclosing their HIV status, only 29% reported feeling that they had the knowledge and skills to challenge HIV related stigma. But for the few who felt able to, disclosing their status had helped their relationships with loved ones, improved their HIV management and inspired them to support other young people living with HIV.
77% of young people reported financial difficulties as a major life stressor, over HIV-related stressors such as stigma. However, 85% believed that the mental health of young people living with HIV was worse than that of their peers not living with HIV.
28% of young people reported being verbally abused or ridiculed because of their HIV status and 20% reported rejection by their spouse or romantic partner due to their HIV status. Other reported stressors included rejection by family members, denial of health services, exclusion from social events and refusal of employment based on their HIV status.
Addressing HIV stigma was one of the most common suggestions for what can be done to improve the mental health of young people living with HIV: “Improve the normalization of HIV with respect to reducing the social stigma surrounding it and the prejudice and disinformation of society” (Young person living with HIV, Americas)
74% of young people living with HIV reported that they did not feel there was adequate funding for mental health support and services in their country and 72% did not know if there were mental health services available to them or where to access them.
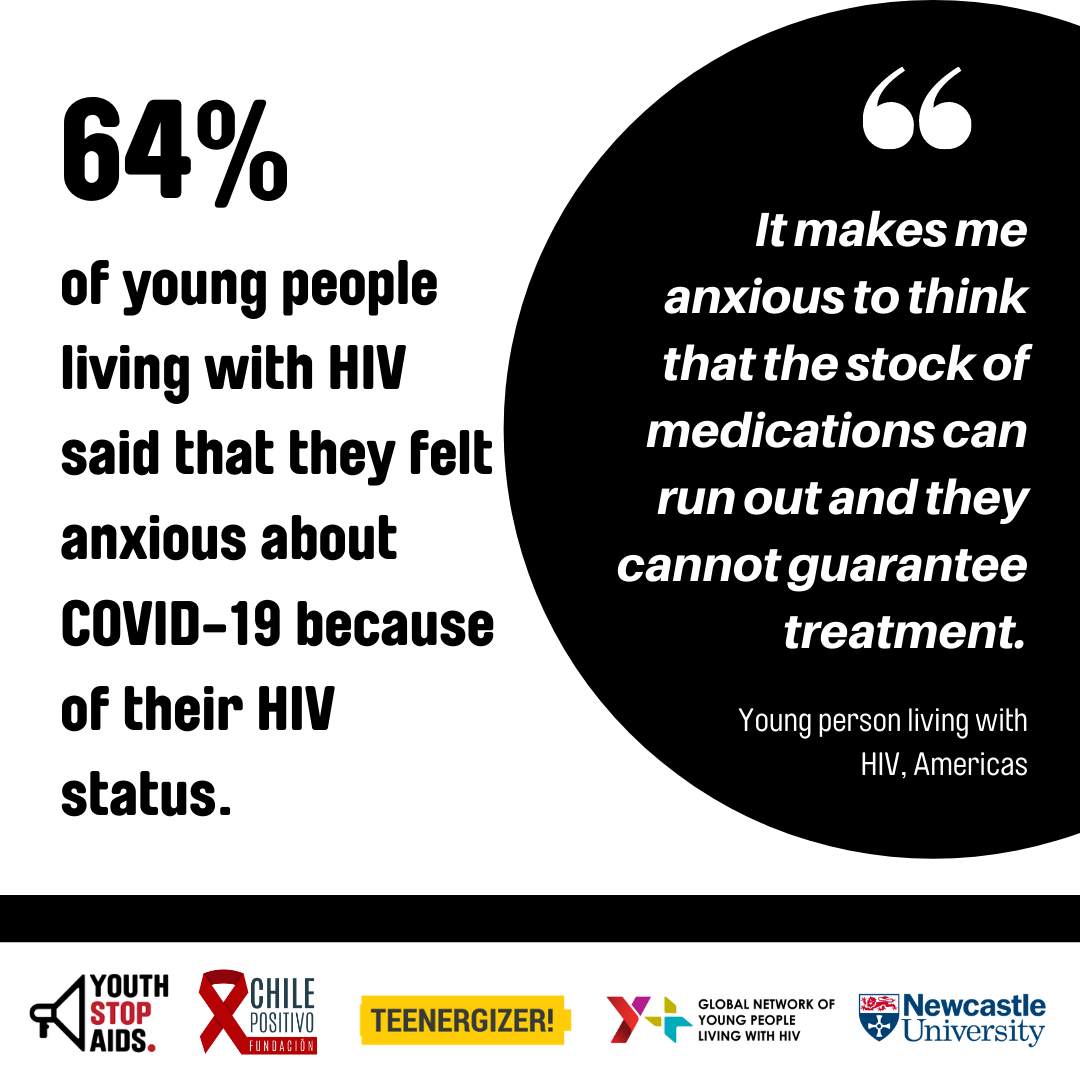
64% of young people living with HIV said that they felt anxious about COVID-19 because of their HIV status.
Our recommendations:
Prioritise and invest in mental health.
Ensure that funding for mental health services for young people living with HIV is sufficient, sustainable and accessible and led by real need, especially in the context of COVID-19. In particular, we recommend the integration of mental health services into existing HIV services and programmes. Young people need to be made aware of which services and support are available to them.
Meaningfully engage young people living with HIV in the mental health and HIV responses.
Young people have an important role to play in the HIV response especially in addressing stigma, facilitating access to mental health services through peer referrals and delivering mental health services. Young people themselves are best placed to understand and address the challenges that they and their peers face. They need to be provided with the support, tools and training to challenge HIV and mental health related stigma. Youth-led organisations need recognition and funding to deliver direct support and facilitate access to youth friendly mental health services.
Understand and address the link between trauma and HIV, and address HIV stigma.
Young people living with HIV experience both HIV and non-HIV related life stressors and traumas. HIV services need to take into account the intersection between HIV and experiences of trauma by adopting a trauma-informed approach to care. This approach would help to facilitate discussions around mental health within HIV services, including stigma, which emerged as one of the most significant HIV-related stressors. Effort should be put into challenging stigma within healthcare settings by addressing poor mental health and HIV understanding, for example through awareness training for healthcare workers.
What next?
We would like to thank everyone who contributed to the research and invite you to watch this space! We will be sharing more results from the survey on this page including a summary report, in early-mid 2021.
We hope that this research not only addresses key knowledge gaps but also inspires action. We believe that we can improve the mental health of young people living with HIV if we listen to young people and work together to adopt the research recommendations.
If you have any questions, would like to request a copy of the full length report or would like to learn more, get in touch with Nadege or Molly:
Nadege Sandrine Uwamahoro, PhD candidate and campaigner with the Youth Stop AIDS student society at Newcastle University, N.S.Uwamahoro2@newcastle.ac.uk
Molly Pugh-Jones, London and Southern England Co-ordinator, Youth Stop AIDS Steering Committee, ysasouthernenglandcoordinator@gmail.com
In partnership with Fundación Chile Positivo, you can access this information in Spanish via their blog post which will go live on World Mental Health Day, 10th October 2020.
In partnership with Teengergizer you can find a Russian translation of this webpage here.
*In total 214 responses were collected; 166 from young people living with HIV and 48 from stakeholders including researchers (13%), advocates/activists (22%) and health workers (39%).
**The survey results are not representative of young people living with HIV globally as they primarily capture views of urban dwelling (91%), highly educated (84% with/undertaking a college degree or above), male including transgender men (68%), Latin Americans (68%), with internet access as due to COVID-19 restrictions the survey was only distributed online. These sample characteristics suggest that the identified challenges and barriers might be harder to overcome for the majority of socioeconomically disadvantaged young people living with HIV. This demographic were underrepresented in the study.
The sample of stakeholders (as listed above) primarily represented the African region (33%), and health providers (39%), working for NGOs (48%) with young people living with HIV aged between 20-24 years (81%).
Many of the barriers to good mental health that were identified were common across regions, although country-level differences were found in some cases. Contextual factors appeared to explain not the barriers themselves, but the degree and form in which they manifested. Also, while the sample size was small, having both quantitative data and rich textual responses proved incredibly insightful.
